The NHS has undergone some pretty major changes over the years, adapting (or failing to adapt, in many cases) to new challenges, technologies, and societal needs.

Some practices and systems that were once routine have now become relics of the past. Much of this is down to decreased funding and not enough staff. However, some things have changed simply because we know more about healthcare and are more efficient these days. Here’s a look at what’s changed.
1. Bedside paper charts

Gone are the days when doctors and nurses would jot down patient information on paper charts hanging at the end of the bed. Electronic Health Records (EHRs) have replaced them, streamlining access to patient data. While digital systems are more efficient, the charm of handwritten notes is long gone.
2. Long-term hospital stays for minor conditions.

Decades ago, patients might have stayed in the hospital for weeks for relatively minor issues. Now, the focus is on same-day discharge or community-based care to free up beds and reduce costs. While this speeds up recovery for many, it also puts more responsibility on outpatient services.
3. The dominance of matrons.

Matrons, with their unmistakable authority and presence, used to be the backbone of hospital wards. While modern nursing leaders have taken their place, the iconic figure of the matron as a hands-on ward manager is a thing of the past. Today’s NHS emphasises multidisciplinary teams over centralised figures.
4. Smoking in hospital wards.

It’s hard to imagine now, but there was a time when smoking wasn’t just permitted in hospitals—it was common. Patients and even staff could light up indoors. Today, strict no-smoking policies reflect modern understanding of health risks, making hospitals smoke-free zones inside and out.
5. Doctor-led care in every step.

Historically, doctors made every key decision about patient care, while nurses followed orders. Now, nurses, pharmacists, and allied health professionals play a more significant role, with advanced practice nurses even prescribing medications. This shift has created a more collaborative healthcare model.
6. General wards separated strictly by gender.

Decades ago, strict gender segregation was standard in hospital wards, even for non-critical conditions. Today, mixed-gender wards are more common due to bed shortages and logistical challenges, though this remains a controversial topic for patient privacy and comfort.
7. Routine tonsillectomies for children.

Once a rite of passage for many children, tonsillectomies were frequently performed for recurring sore throats or tonsillitis. Modern guidelines recommend more conservative treatments, reserving surgery for severe, persistent cases. Fewer tonsillectomies mean less disruption for young patients and their families.
8. Overnight stays after childbirth.

Not so long ago, new mothers routinely spent several days in hospital after giving birth. Now, many are discharged within 24 hours if there are no complications. While this promotes recovery at home, it can leave some new parents feeling rushed and unsupported.
9. Routine use of pagers for staff communication.
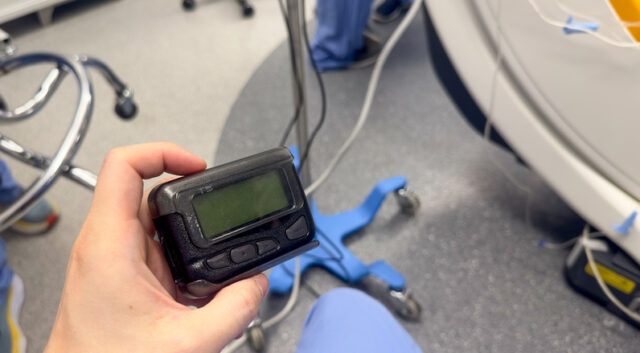
Pagers were once the primary way to contact on-call doctors and nurses. While they haven’t disappeared entirely, smartphones and secure messaging apps are quickly taking their place. Digital communication is faster and more versatile, but some staff still value the simplicity of a pager beep.
10. Free parking at hospitals.

Free parking was once common at NHS hospitals, but now many charge fees to fund maintenance and infrastructure. This has become a contentious issue, especially for regular visitors and staff who argue that healthcare access shouldn’t come with added costs.
11. Open visiting hours.

Decades ago, visiting hours in hospitals were more flexible, allowing family and friends to drop in regularly. Now, most hospitals have stricter schedules and limits, particularly after the pandemic, which emphasised the need for infection control. This shift has left some patients feeling more isolated.
12. Local GP surgeries providing 24-hour care.

There was a time when your local GP surgery offered round-the-clock care, with doctors personally attending to emergencies. Today, out-of-hours services are centralised, and patients are directed to NHS 111 or urgent care centres. While efficient, this change has distanced patients from their personal GPs.
13. Prescription charges being minimal or non-existent

In the early days of the NHS, prescriptions were free for everyone. Over time, charges were introduced and have steadily increased to the current £9.90. While exemptions exist for certain groups, many patients now face significant costs for routine medications, a stark contrast to the system’s original intent.




